Summary
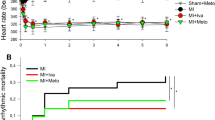
The effect of intracoronary (IC) pretreatment with different calcium antagonists (diltiazem, nifedipine, verapamil) on the development of infarcts was investigated in two experimental series including 35 open-chest pigs. The left anterior descending coronary artery (LAD) was distally ligated for 75 minutes (series A) or for 45 minutes (series B) and was reperfused for 24 hours. Infarct size was determined as the ratio of infarcted myocardium (tetrazolium stain) to the risk region (dye technique). In series A, 20 pigs were pretreated immediately before occlusion with either IC diltiazem (n=5, 4 mg/2 min), IC nifedipine (n=5, 0.4 mg/2 min), IC verapamil (n=5, 1 mg/2 min), or isotonic sodium chloride solution (n=5). In series B, IC diltiazem (n=5, 4 mg/2 min), IC verapamil (n=5, 1 mg/2 min), or isotonic saline solution (n=5) were administered 8 minutes prior to ischemia. The IC infusion of all calcium antagonists (series A) depressed left ventricular peak pressure, diastolic blood pressure, and dp/dt max and increased heart rate and coronary venous oxygen saturation. The development of infarcts was significantly delayed by IC diltiazem and IC verapamil. Mean infarct sizes (series A) amounted to 62% in the diltiazem group, 88% in the nifedipine group, 40% in the verapamil group, and 94% in the control group. In series B, where a time period of 8 minutes elapsed between pretreatment and induction of ischemia, mean infarct sizes after 45 minutes of ischemia and 24 hours of reperfusion amounted to 47% in the diltiazem group, 4% in the verapamil group, and 76% in control experiments. The better protection of verapamil in series B can mainly be ascribed to its longer lasting regional depression compared to diltiazem.
In conclusion, at the given drug concentrations, IC verapamil and IC diltiazem enhanced the ischemic tolerance to a greater extent than IC nifedipine (series A). When a time period of 8 minutes had elapsed between IC treatment and the onset of ischemia (series B), verapamil still exhibited a protective effect on the treated myocardium, which can mainly be ascribed to its long-lasting negative inotropic action.
Similar content being viewed by others
References
Serruys, PW, van denBrand, M, Brower, RW, Hugenholtz, PG. Regional cardioplegia and cardioprotection during transluminal angioplasty, which role for nifedipine?. Eur Heart J 1983;4:suppl C:115–121.
Hombach, V, Höpp, HW, Behrenbeck, DW, Fuchs, M, Osterspey, A, Hilger, HH. Ischämietoleranz unter intrakoronar verabreichtem Nifedipin während transluminaler Koronarangioplastie. In: Meyer, J, Erbel, R (eds.) Intravenöse und Intrakoronare Anwendung von Adalat. Berlin, New York, Tokyo, Springer Verlag 1985:80–88.
Kober, K, Kästner, R, Hopf, R, Kaltenbach, M. Die direkte myokardiale antiischämische Wirkung von Diltiazem beim Menschen. Z Kardiol 1986;75:386–393.
Zalewski, A, Goldberg, S, Dervan, JP, Slysh, S, Maroko, PR. Myocardial protection during transient coronary artery occlusion in man: Beneficial effects of regional beta-adrenergic blockade. Circulation 1986;73:734–739.
Dorros, G, Cowley, MJ, Simpson, J, Bentiroglio, LG, Block, KPL, Bourassa, M, Dere, K, Gosselin, AJ, Grüntzig, AR, Kelsey, SF, Kent, KM, Mock, MB, Mullin, SM, Myler, RK, Passami, ER, Sterzer, SH, William, DO. Percutaneous transluminal coronary angioplasty: Report of complications from the National Heart, Lung and Blood Institute PTCA registry. Circulation 1983;67:723–730.
Shin, MF, Siverton, NP, Oeleley, D, Cumberland, D. Acute coronary occlusion during percutaneous transluminal coronary angioplasty. Br Heart J 1985;54:129–133.
Killen, DA, Hamaker, WR, Reed, WA. Coronary artery bypass following percutaneous transluminal coronary angioplasty. Ann Thorac Surg 1985;40:133–138.
Klepzig, HJr, Schraub, J, Huber, H, Hör, G, Kober, G, Satter, P, Kaltenbach, M. Aortokoronare bypass-operation als Notfalleingriff nach transluminaler koronarer Angioplastik. Dtsch Med Wschr 1986;111:737–741.
Klein, HH, Pich, S, Lindert, S, Buchwald, A, Nebendahl, K, Kreuzer, H. Intracoronary superoxide dismutase for the treatment of reperfusion injury. A randomized placebocontrolled blinded trial in ischemic, reperfused porcine hearts. Basic Res Cardiol 1988;83:141–148.
Klein, HH, Pich, S, Bohle, RM, Lindert, S, Nebendahl, K, Buchwald, A, Schuff-Werner, P, Kreuzer, H. The anti-inflammatory agent BW 755 C in ischemic, reperfused porcine hearts. J Cardiovasc Pharmacol, 1988;12:338–344.
Nachlas, MU, Shnitka, TK. Macroscopic identification of early myocardial infarcts by alteration in dehydrogenas activity. Am J Pathol 1963;42:379–405.
Bugge-Asperheim, B, Leraand, S, Kill, F. Local dimensional changes of the myocardium measured by ultrasonic technique. Scand J Clin Lab Invest 1969;24:361–371.
Theroux, P, Franklin, D, Ross, JJr, Kemper, WS. Regional myocardial function during acute coronary artery occlusion and its modification by pharmacologic agents in the dog. Circ Res 1974;35:896–908.
Heimisch, W, Hagl, S, Gebhardt, K, Meisner, H, Mendler, N, Sebening, F. Direct measurement of cyclic changes in regional wall geometry in the left ventricle of the dog. Innov Tech Biol Med 1981;2:487–501.
Freeman, GL, LeWinter, NM, Engler, RL, Covell, JW. Relationship between myocardial fiber direction and segment shortening in the midwall of the canine left ventricle. Cir Res 1985;56:31–39.
Schaper, W, Frenzel, H, Hort, W. Experimantal coronary artery occlusion. I. Measurement of infarct size. Basic Res Cardiol 1979;74:46–53.
Klein, HH, Puschmann, S, Schaper, J, Schaper, W. The mechanism of the tetrazolium reaction in identifying experimental myocardial infarction. Virchows Arch (Path Anat) 1981;393;287–297.
Pich, S, Klein, HH, Lindert, S, Nebendahl, K, Kreuzer, H. Cell death in ischemic, reperfused porcine hearts: A histochemical and functional study. Basic Res Cariol, 1988;83:550–559.
Eckstein, RW. Coronary interarterial anastomoses in young pigs and mongrel dogs. Circ Res 1954;2:460–465.
Sjöquist, PO, Duker, G, Almgren, O. Distribution of the collateral blood flow at the lateral border of the ischemic myocardium after acute coronary occlusion in the pig and the dog. Basic Res Cardiol 1984;79:164–175.
Klein HH, Pisch S, Lindert S, Nebendahl K, Kreuzer H. The effect of intracoronary diltiazem on regional myocardial function and development of infarcts in porcine hearts. Res Exper Med, in press.
Kloner, RA, Braunwald, E. Effects of calcium antangonists on infarcting myocardium. Am J Cardiol 1987;59:84B-94B.
Nayler, WG, Panagiotopoulos, S, Elz, JS, Sturrock, WJ. Fundamental mechanisms of action of calcium antagonists in myocardial ischemia. Am J Cardiol 1987;59:75B-83B.
Marokko, PR, Kjekshus, JR, Sobel, BE, Watanabe, T, Covell, JU, Ross, JJr, Braunwald, E. Factors influencing infarct size following coronary artery occlutions. Circulation 1971;43:67–82.
Schaper, W, Binz, K, Sass, S, Winkler, B. Influence of collateral blood flow and of variations in MVO2 on tissue-ATP content in ischemic and infarcted myocardium. J Mol Cell Cardiol 1987;19:19–37.
Walsh, RA, Badke, FR, O'Rourke, RA. Differential effects of systemic and intracoronary calcium channel blocking agents on global and regional left ventricular function in conscious dogs. Am Heart J 1981;102:341–350.
Bertrand, ME, Dupuis, BA, Lablanche, JM, Tilmant, PY, Thieuleux, FA. Coronary hemodynamics following intravenous or intracoronary injection of diltiazem in man. J Cardiovasc Pharmacol 1982;4:695–699.
Serruys, PW, Hooghoudt, TEH, Reiber, JHC, Slager, C, Brower, RW, Hugenholtz, PG. Influence of intracoronary nifedipine of left ventricular function, coronary vasomotility, and myocardial oxygen consumption. Br Heart J 1983;49:427–441.
Ferlinz, J, Stavens, CS. Regional and global responses in coronary blood flow and exercise tolerance after intracoronary versus intravenous verapamil administration in coronary artery disease (abstr). J Am Coll Cariol 1984;3:578.
Walsh, RA, O'Rourke, RA. Direct and indirect effects of calcium entry blocking agents on isovolumic left ventricular relaxation in conscious dogs. J Clin Invest 1985;75:1426–1434.
Watts, JA, Maiorano, LJ, Maiorano, PC. Comparison of the protective effects of verapamil, diltiazem, nifedipine, and buffer containing low calcium upon global myocardial ischemic injury. J Mol Cell Cardiol 1986;18:255–263.
Kohlhardt, M, Wais, U. Quantitative differences between the inhibitory action of verapamil and Ni ions on the slow response action potential in mammalian ventricular myocardium. J Mol Cell Cardiol 1979;11:917–921.
Molyvdas, P-A, Sperelakis, N. Comparison of the effects of several calcium antagonistic drugs on the electrical activity of guinea pig Purkinje fibers. Eur J Pharm 1983;88:205–214.
Amende, I, Simon, R, Hood, WPJr, Hetzer, R, Lichtlen, PR. Intracoronary nifedipine in human beings: Magnitude and time course of changes in left ventricular contraction/relaxation and coronary sinus blood flow. J Am Coll Cardiol 1983;2:1141–1145.
Buffalo, E, Andrade, JCS, Succi, JE, Leao, LEV, Cueva, C, Branco, JN, Carvalho, ACC, Galuuci, C. Direct myocardial revascularization without extracorporeal circulation: Technique and initials results. Texas Heart Institute J 1985;12: 33–41.
Author information
Authors and Affiliations
Additional information
This study was supported by a grant from the Deutsche Forschungs-gemeinschaft, SFB 330 Organprotektion. The paper contains parts of the “Habilitationschrift” of Dr. H. H. Klein.
Rights and permissions
About this article
Cite this article
Klein, H.H., Pich, S., Lindert, S. et al. Comparative study on the enhancement of ischemic tolerance by intracoronary pretreatment with three calcium antagonists in pig hearts. Cardiovasc Drug Ther 2, 815–821 (1989). https://doi.org/10.1007/BF00133213
Issue Date:
DOI: https://doi.org/10.1007/BF00133213