Abstract
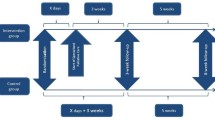
The assessment of physical symptoms is a key com-ponent of quality of life studies in palliative care, but is often hampered by missing data from patient-completed questionnaires. In two large multicentre randomized trials of palliative treatment conducted by the Medical Research Council Lung Cancer Working Party, involving over 700 patients, patients completed Rotterdam Symptom Checklists and doctors reported on eleven of the same physical symptoms at each assessment, using the same 4-point severity scale. Ratings by doctors and patients were compared with respect to compliance, severity, and outcomes for the respective trials. Doctors provided more data than patients: 66% vs. 52%in the first 6 months in one trial, 68% vs. 61% in the other. Comparisons of over 33,000 symptom assessments showed 78% complete agreement between doctor and patient, 18% disagreement by one, 4% two, and 1% three grades (complete disagreement). There was no change in levels of agreement over time, but increasing disagreement with increasing symptom severity, and a consistent bias towards doctors underestimating severity. Nevertheless, the two methods of data collection resulted in similar between-treatment conclusions. Therefore, in randomized trials the doctors' assessments of key physical symptoms may be sufficient for the between-treatment comparison. However, the fact that doctors underestimate symptom severity 15% of the time has important implications for palliative interventions.
Similar content being viewed by others
References
Ganz PA, Schag CAC, Lee JJ, Sim MS. The CARES: a generic measure of health-related quality of life for patients with cancer. Qual Life Res 1992; 1: 19-29.
Aaronson NK, Ahmedzai, S, Bergman B, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: A Quality of Life Instrument for use in International Clinical Trials in Oncology. JNCI 1993; 85: 365-376.
Cella DF, Bonomi AE, Lloyd SR, Tulsky DS, Kaplan E, Bonomi P. Reliability and validity of the Functional Assessment of Cancer Therapy -Lung (FACT-L) quality of life instrument. Lung Cancer 1995; 12: 199-220.
Schipper H, Clinch J, McMurray A, Levitt M. Measuring the quality of life of cancer patients: The functional living index-cancer: Development and validation. J Clin Oncol 1984; 2: 472-483.
De Haes JCJ, Knippenberg FCE, Neijt JP. Measuring psychological and physical distress in cancer patients: structure and application of the Rotterdam Symptom Checklist. Br J Cancer 1990; 62: 1034-1038.
Hopwood P, Stephens RJ, Machin D. Approaches to the analysis of quality of life data: experiences gained from a Medical Research Council Lung Cancer Working Party palliative chemotherapy trial. Qual Life Res 1994; 3: 339-352.
Sprangers MAG, Aaronson NK. The role of health care providers and significant others in evaluating the quality of life of patients with chronic disease: A review. J Clin Epid 1992; 45: 743-760.
Slevin ML, Plant H, Lynch D, Drinkwater J, Gregory WM. Who should measure quality of life, the doctor or the patient? Br J Cancer 1988; 57: 109-112.
Spitzer WO, Dobson AJ, Hall J, Chesterman E, Levi J, Shepherd R, Battista RN, Catchlove BR. Measuring the quality of life of cancer patients. A concise QL-index for use by physicians. J Chron Dis 1981; 34: 585-597.
Ganz PA, Schag CAC, Cheng HL. Assessing the quality of life - A study in newly-diagnosed breast cancer patients. J Clin Epid 1990; 43: 75-86.
Presant CA. Quality of life in cancer patients. Who measures what? Am J Clin Oncol 1984; 7: 571-573.
Medical Research Council Lung Cancer Working Party. Randomised trial of four-drug versus less intensive two drug chemotherapy in the palliative treatment of patients with small cell lung cancer (SCLC) and poor prognosis. Br J Cancer 1996; 73: 406-413.
Medical Research Council Lung Cancer Working Party. Randomized trial of palliative two-fraction versus more intensive 13-fraction radiotherapy for patients with inoperable non-small cell lung cancer and good performance status. Clin Oncol 1996; 8: 167-175.
World Health Organization. WHO Handbook for Reporting Results of Cancer Treatment.Geneva, Switzerland: WHO Offset Publication No. 48, 1979.
Medical Research Council Lung Cancer Working Party. Inoperable non-small cell lung cancer (NSCLC): a Medical Research Council randomised trial of palliative radiotherapy with two fractions or ten fractions. Br J Cancer 1991; 63: 265-270.
Medical Research Council Lung Cancer Working Party. A Medical Research Council (MRC) randomised trial of palliative radiotherapy with two fractions or a single fraction in patients with inoperable non-small cell lung cancer (NSCLC) and poor performance status. Br J Cancer 1992; 65: 934-941.
Stephens RJ, Hopwood P. Response to palliative treatment: the case for a standard definition. Psycho-Oncology 1996; 5(Suppl 3): 13 [Abstract].
Hopwood P, Stephens RJ. Symptoms at presentation for treatment in patients with lung cancer: Implications for the evaluation of palliative treatment. Br J Cancer 1995; 71: 633-636.
Epstein AM, Hall JA, Tognetti J, Son LH, Conant L. Using proxies to evaluate quality of life. Can they provide valid information about patients' health status and satisfaction with medical care? Med Care 1989; 27: S91-S98.
Ford S, Fallowfield L, Lewis S. Can oncologists detect distress in their out-patients and how satisfied are they with their performance during bad news consultations? Br J Cancer 1994; 70: 767-770.
Grossman SA, Sheidler VR, Swedeen K, Mucenski J, Piantadosi S. Correlation of patient and caregiver ratings of cancer pain. J Pain Sympt Manag 1991; 6: 53-57.
Au E, Loprinzi CL, Dhodapkar M, Nelson T, Novotny P, Hammack J, O'Fallon J. Regular use of a verbal pain scale improves the understanding of oncology inpatient pain intensity. J Clin Oncol 1994; 12: 2751-2755.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Stephens, R.J., Hopwood, P., Girling, D.J. et al. Randomized trials with quality of life endpoints: Are doctors' ratings of patients' physical symptoms interchangeable with patients' self-ratings?. Qual Life Res 6, 225–236 (1997). https://doi.org/10.1023/A:1026458604826
Published:
Issue Date:
DOI: https://doi.org/10.1023/A:1026458604826