Abstract
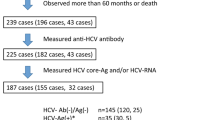
The hepatitis C virus (HCV) may be an important cause of chronic liver disease in renal transplant recipients. We investigated retrospectively the incidence and outcome of HCV infection in long-term renal transplant recipients and patients on hemodialysis. Stored, pretransplant sera of transplant recipients with normal liver biochemistry at surgery were tested for hepatitis C by a second-generation enzyme immunoassay. Hemodialysis patients were tested by a first-generation enzyme-linked immunosorbent assay (ELISA) against c100-3. We studied 252 renal transplant recipients and 58 hemodialysis patients followed for 65±10 months and 26±6 months, respectively. Fifteen percent (38/252) of the transplant recipients were HCV positive as were 3/58 (5%) of the hemodialysis patients. Over liver disease occurred in 22/252 (8.7%) transplant recipients and none in the hemodialysis group. Thirty-six percent (8/22) of transplant recipients with overt liver disease were HCV positive. No HCV-positive patients died of liver failure. Of six biopsies in the HCV-positive transplant group, two had histological evidence of CAH. CAH was seen in six of eight biopsies in the HCV-negative transplants and two of these latter patients progressed to cirrhosis. No hemodialysis patients had clinical or histological evidence of chronic liver disease. Two HCV-negative transplant patients died of liver failure, while no deaths related to liver disease occurred in hemodialysis patients regardless of HCV status. We conclude that hepatitis C may cause chronic hepatitis in renal transplant patients. However, chronic liver disease in HCV-positive renal transplant recipients appears to be a clinically and histologically benign entity. HCV-positive potential renal allograft recipients with normal liver biochemistry should not be excluded from renal transplantation.
Similar content being viewed by others
References
Anuras S, Piros J, Corry R, Boney WW, Forker EL, Colville DS: Liver disease in renal transplant recipients. Arch Intern Med 137:42–48, 1977
Mozes MF, Ascher NL, Najarian JS: Jaundice after renal allo-transplantation. Ann Surg 188:783–790, 1978
Ware AJ, Luby JP, Eigenbrodt EH, Long DL, Hull AR: Spectrum of liver disease in renal transplant recipients. Gastroenterology 68:755–764, 1975
Boyce NW, Holdsworth SR, Hooke D, Thomson NM, Atkins RC: Non-hepatitis-associated liver disease in a renal transplant population. Am J Kidney Dis 11:307–312, 1988
Parfrey PS, Farge D, Guttmann RD, Dandavino R, Kenick S: Chronic hepatitis in end stage renal disease. Comparison of HBsAg negative and HBsAg positive patients. Kidney Int 28:959–967, 1985
Pien FD, Smith TF, Anderson CF, Webel ML, Taswell HF: Herpes virus in renal transplant patients. Transplantation 16:489–495, 1973
Fine RN, Grushkin CM, Malekzadehm M, Wright HT: Cytomegalovirus syndrome following renal transplantation. Arch Surg 105:564–570, 1972
Chang RS, Lewis JP, Reynolds RD, Neuman J, Sullivan MJ: Oropharyngeal excretion of Epstein-Barr virus by patients with lymphoproliferative disorder and recipients of renal homograft. Ann Intern Med 88:34–40, 1978
Sparberg M, Simon M, Del-Greco F: Intrahepatic cholestasis due to azathioprine. Gastroenterology 57:439–441, 1969
Shorey J, Schenker S, Sukilon Combes B: Hepatoxicity of mercaptopurine. Arch Intern Med 122:54–58, 1968
Laquaglia MP, Tolkoff-Rubin NE, Rubin R, Dienstag JL, Cosimi AB, Herrin JT, Kelly M: Impact of hepatitis on renal transplantation. Transplantation 32:504–507, 1981
Briggs WA, Lazarus TM, Birtch AG, Hampers CL, Hager EB, Merrill JP: Hepatitis affecting hemodialysis and transplant recipients: Its considerations and consequences. Arch Intern Med 132:21–28, 1973
Parfrey PS, Forbes RDC, Hutchinson TA, Guttman RD: The prevalence and progression of liver disease in renal transplant recipients. A histological study. Transplant Proc 16:1103–1105, 1984
Pereira BJ, Milford EL, Kirkman RL, Quan S, Sayre KR, Johnson PJ, Wilbur JC, Levy AS: Prevalence of hepatitis C virus rna in organ donors positive for hepatitis C antibody and in recipients of their organs. N Engl J Med 327:910–915, 1992
Roth D, Fernandez JA, Miller J, Burke GW, Esquenazi V: Detection of antibody to hepatitis C virus in renal transplant recipients. Transplantation 51:396–400, 1991
Huang C, Liaw YF, Huang Y: The clinical outcome of hepatitis C virus antibody positive renal allograft recipients. Transplantation 53:763–765, 1992
Stempel CA, Lake J, Kuo G, Vincenti F: Hepatitis C—its prevalence in end-stage renal failure patients and clinical course after kidney transplantation. Transplantation 55:273–276, 1993
Marcen R, Pascual J, Ortuno J, Fernandez-Munoz R, Teruel JL, Lian OF, Celma ML: Hepatitis C virus infection in kidney transplant patients. Transplant Proc 24:87–88, 1992
Ponz E, Campistol JM, Andreu J, Bruguera M, Barrera JM, Gil C, Pinto JB: Hepatitis C virus infection among kidney transplant recipients. Kidney Int 40:748–751, 1992
Lam KC, Trepo C, Wu PC: Deleterious effect of prednisolone in HBsAg positive chronic active hepatitis. N Engl J Med 304:380–386, 1981
Hoofnagle JH, Dusheiko GM, Schafer DF, Jones EA, Micetich KC, Young RC, Costa J: Reactivation of chronic hepatitis B virus infection by cancer chemotherapy. Ann Intern Med 96:447–449, 1982
Dusheiko G, Song E, Bowyer S, Whitcutt M, Mair G, Meyers A, Kew MC: Natural history of hepatitis B virus infection in renal transplant recipients—a fifteen year follow-up. Hepatology 3:330–336, 1983
Weiner AJ, Kuo G, Bradley DW, Choo QL, Bonino F, Saracco G, Lee L, Rosenblat J, Houghton M: Detection of hepatitis C viral sequences in non-A, non-B hepatitis. Lancet 335:1–3, 1990
Degos F, Degott C, Bedrossian J, Camiliert JP, Barbanel C, Dubost A, Rueff B, Benhamou JP, Kreis H: Is renal transplantation involved in post transplant liver disease. Transplantation 29:100–102, 1980
Wolf PL, William D, Coplom H, Coulson AS: Low aspartate transaminase activity in serum of patients undergoing chronic hemodialysis. Clin Chem 18:567–568, 1972
Pereira BJG, Milford EL, Kirkman RL, Sayre KR, Johnson PJ, Wilber JC, Quan S, Levey AS: Prevalence of HCV RNA in hepatitis C antibody positive cadaver organ donors and recipients of organs from these donors. Transplantation 1994 (in press)
Author information
Authors and Affiliations
Additional information
Presented in abstract form (Gastroenterology 102:A830, 1992) at the American Gastroenterological Association, April 1992.
Rights and permissions
About this article
Cite this article
Kazi, S., Prasad, S., Pollak, R. et al. Hepatitis C infection in potential recipients with normal liver biochemistry does not preclude renal transplantation. Digest Dis Sci 39, 961–964 (1994). https://doi.org/10.1007/BF02087544
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF02087544