Abstract
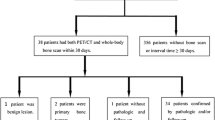
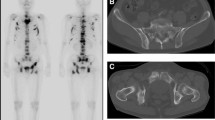
Seventy-seven adult patients with suspected skeletal metastases were divided into two groups. In group A (n=30), following intravenous administration of 20 mCi (740 MBq) of technetium-99m methylene diphosphonate (99mTc-MDP), 3- and 24-h scintigraphy of bone lesions was performed. The 24/3 h lesion to bone background radiouptake ratio (RUR) was calculated for each lesion. In group B (n=47), the same procedure was followed with dexamethasone intervention (10 mg in 24 h) following the 3-h acquisition. In group A, after determination of the critical point, malignant and degenerative bone lesions could be separated with a sensitivity, specificity and accuracy of 0.76, 0.72 and 0.73, respectively. The mean RUR of the malignant lesions was 1.20± 0.23, and that of the benign lesions, 0.95± 0.15. In group B cases, significantly increased sensitivity, specificity and accuracy of 0.87, 0.94 and 0.92, respectively, were found (P<0.001). The mean RUR of the malignant lesions was 1.48± 0.34, and that of degenerative lesions, 0.88± 0.19. Dexamethasone interventional bone scintigraphy seems to be a new cost-effective method for differentiating malignant from degenerative bone lesions using the RUR.
Similar content being viewed by others
References
Boland PJ, Lane JM, Sudarshan N, et al. Metabolic disease of the spine. Clin Orthop 1982; 109: 95–99.
Osmond JD, Pendergrass HP, Potsaid MS. Accuracy of 99m Tc-diphosphonate bone scans and roentgenograms in detection of prostate, breast and lung carcinoma metastases. AJR 1975;124: 972–979.
Rosenberg RD, Mettler FA, Christie JH. The radionuclide bone scan in malignant disease. In: Mettler FA, ed. Radionuclide bone imaging and bone densitometry. New York: Churchill Livingstone; 1988: 63–86.
Guan S, Chu L, Hwang W, Chen W. The differential diagnosis of benign and malignant bony lesions in bone scanning. Clin Nucl Med 1990; 15: 424–427.
Arnstein NB, Harbert JC, Byrne PJ. Efficacy of bone and liver scanning in breast cancer patients treated with adjuvant chemotherapy. Cancer 1984; 54: 2243–2247.
Gold RH, Basset LW, Radionuclide evaluation of skeletal metastases: practical considerations. Skeletal Radiol 1986; 15: 1–9.
Perez DJ, Milan J, Ford HT, et al. Detection of breast carcinoma metastases in bone: relative merits of X-rays and skeletal scintigraphy. Lancet 1983;II: 613–616.
Kunkler IH, Merrick MV, Rodger A. Bone scintigraphy in breast cancer: a nine year followup. Clin Radiol 1985; 36: 279–282.
Israel O, Front D, Frenkel A, Klienhaus U. 24-hour/4 hour ratio of technetium-99m methylene disphosphonate uptake in patients with bone metastases and degenerative bone changes. J Nucl Med 1985; 26: 237–240.
Kashyap R, Bhatnagar A, Mondal A, Sawroop K. 24/3 Hour radio-uptake technique for differentiating degenerative and malignant bone lesions in bone scintigraphy. Australas Radiol 1993;37: 198–200.
Jacobson AF, Stomper PC, Jochelson MS, et al. Association between number and sites of new bone abnormalities and presence of skeletal metastases in patients with breast cancer. J Nucl Med 1990; 31: 387–392.
Silberstien EB, Gelfond MJ, Muroff LR. Bone scintigraphy in primary osseous neoplasia and invasive marrow disorders of adults. In: Silberstien EB, ed. Bone scintigraphy. Mt. Kisco, N.Y.: Futura; 1984: 259.
Frankel DG, Daffner RH, Wang SE. Disseminated tuberculosis. Skel Radiol 1991; 20: 130–133.
Fordham EW, Ali A, Turner DA, et al. Inflammatory disease. In: Atlas of total body radionuclide imaging. New York: Harper & Row; 1982: 396–425.
Elgazzar AH, Abdel Dayem HM, Shible O, Brucellosis simulating metastases on Tc-99m MDP bone scan. Clin Nucl Med 1991; 16: 189–191.
Corconan RJ, Thrall JH, Kyle RW et al. Solitary abnormalities in bone scans of patients with extraosseous malignancies. Radiology 1976; 121: 663–667.
Collins JD, Basset L, Main GD, et al. Percutaneous biopsy following positive bone scans. Radiology 1979; 132: 439.
Schirazi RH, Rayadu GVS, Fordham EW. Review of solitary 18-F bone scan lesions. Radiology 1974; 112: 369–372.
Edeiken J. Radiological approach to diagnosis of bone disease. In: Goswitz FA, Andrews GA, Viomonte M, eds. Clinical use of radionuclides: critical comparison with other techniques. Washington DC: USAEC; 1972: 90–100.
Schutte HE. The influence of bone pain on the results of bone scan. Cancer 1979; 44: 2039.
Fordham EW, Ali A. Skeletal imaging in malignant disease. In Gottschalk A, Hoffer PB, Potchen EJ, eds. Diagnostic nuclear medicine. Baltimore: Williams and Wilkins; 1988: 1011–1032.
O'Mara RE. Benign bone disease. In: Gottschalk A, Hoffer PB, Potchen EJ, eds. Diagnostic nuclear medicine. Baltimore: Williams and Williams; 1988: 1033–1075.
Feig SA. Imaging techniques and guidelines for evaluation and follow-up of breast cancer patients. CRC Crit Rev Diagn Imaging 1987; 27: 1–16.
Podoloff DA, Kim EE. ‘Sub’-Superscan: manifestation of bone marrow metastases? Clin Nucl Med 1989; 14: 597–602
Gold RI, Seeger LL, Bassett LW, Steckel RJ. An integrated approach to the evaluation of metastatic bone disease. Radiol Clin North Am 1990; 28: 471–483.
Smoker WRK, Godersky JC, Knutzone RK, et al. MR imaging in evaluating metastatic spinal disease. AJNR 1987; 8: 901–905.
Murphy WA. Imaging bone tumours in the 1990's. Cancer 1991; 67: 1169–1176.
Bates D, Ruggieri P. Imaging modalities for evaluation of spine. Radiol Clin North Am 1991; 29: 675–690.
Frank JA, Ling A, Patronas NJ, et al. Detection of malignant bone tumours: MR imaging vs scintigraphy. Am J Roentgenol 1990; 155: 1043–1048.
Watt I. Musculoskeletal system. In: Davies ER, Thomas WEG, eds. Nuclear medicine: applications to surgery. Kent, UK.: Castle House; 1988: 219–253.
Bocking A. Cytological vs. histological evaluation of percutaneous biopsy. Cardiovasc Intervent Radiol 1991; 14: 5–12.
Citrin DL, Bessent RG, McGinley E, et al. Dynamic studies with Tc-99m HEDP in normal subjects and in patients with bone tumors. J Nucl Med 1975; 16: 886–890.
Castronovo FP, McKusick KA, Strauss HW. The 4 h/24 h 99mTc-MDP whole body retention: a new index in bone pathology. Nucl Med Biol 1986; 13(6): 599–602.
Eisenhut M. Iodine 131 labeled diphosphonates for the palliation of bone metastases. 1. Organ distribution and kinetics of I-131-BDP 3 in rats. J Nucl Med 1984; 25: 1356–1361.
Eisenhut M, Berberich R, Kimming B, Oberhausen E. Iodine 131 labeled diphosphonates for palliation of bone metastases. 11. Preliminary results with iodine-131 BDP 3. J Nucl Med 1986; 27: 1255–1261.
Galasko CBS. Editorial: mechanism of uptake of bone imaging isotopes by skeletal metastases. Clin Nucl Med 1980; 5: 565–568.
Galasko CBS. Bone metastases studies in experimental animals. Clin Orthop Rel Res 1982; 169: 269–285.
Garcia JF. Bone growth and metabolism. In: Mettler FA, ed. Radionuclide bone imaging and densitometry. New York: Churchill Livingstone; 1988: 1–12.
Burkhardt R, Frisch B, Schlag R, Sommerfeld W. Carcinomatous osteodysplasia. Skel Radiol 1982; 8: 169.
Guyton A. Text Book of medical physiology, 7th edn. Philadelphia: Saunders; 1986: 937–953.
Mettler FA, Monsein L, Rosenberg RD. Radionuclides and normal bone scan. In: Mettler FA, ed. Radionuclide bone imaging and densitometry. New York: Churchill Livingstone, 1988: 13–29.
Charkes ND. Skeletal blood flow: implications for bone scan interpretation. J Nucl Med 1980; 21: 91–98.
Thrall JH, Geslien GE, Corcoran RJ, Johnson MC. Abnormal radionuclide deposition patterns adjacent to focal skeletal lesions. Radiology 1975; 115: 659–663.
Hughes SPF, Davies R, Khan RA, Kelly P. Fluid space in bone. Clin Orthop 1978; 134: 332–341.
Schwartz Z, Shani J, Soskolne WA, et al. Uptake and biodistribution of technetium-99m MDP during rat tibial bone repair. J Nucl Med 1993; 34: 104–108.
Williams GH, Dluhy RG. Diseases of the adrenal cortex. In: Harrison's principles of internal medicine, 10th edn. Singapore: McGraw Hill, 1983.
Author information
Authors and Affiliations
Additional information
Correspondence to: A. Bhatnagar
Rights and permissions
About this article
Cite this article
Bhatnagar, A., Mondal, A., Kashyap, R. et al. Differentiation of malignant and degenerative bone lesions using dexamethasone interventional 3- and 24-hour bone scintigraphy. Eur J Nucl Med 21, 609–614 (1994). https://doi.org/10.1007/BF00285582
Received:
Revised:
Issue Date:
DOI: https://doi.org/10.1007/BF00285582