Abstract
Purpose. The objectives of this study were to 1) construct a pharmacokinetic-pharmacodynamic (PK-PD) model, and 2) determine the PKs and PDs of (R)-albuterol when given by nebulization to 8 dogs for 7 consecutive days.
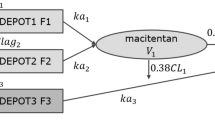
Methods. Four doses were evaluated (0.002, 0.02, 0.1, and 0.4 mg/kg/day). Blood samples were obtained after drug administration on days 1 and 7. Heart rates (HR) were obtained during treatment days 1, 4 and 7. All (R)-albuterol plasma concentrations were fitted using a mixed gut-lung absorption 2-compartment PK model. Day-1, 4, and 7 HR data were co-modeled using a direct response model with Hill-type equations, including a necessary tolerance phenomenon. The population PK-PD analysis was performed with an iterative 2-stage methodology (IT2S).
Results. No chiral inversion was seen, and double absorption peaks on the plasma concentration versus time curves were observed in the majority of dogs. These were hypothesized to be the result of combined gut and lung absorption of (R)-Albuterol. Results indicated that 67% (range: 57-89%) of (R)-albuterol systemic exposure after nebulized administration is due to gut absorption. Mean population PK parameters were KaGI (10±5.7 h−1), KaLUNG (21±9.5 h−1), CLc/F (0.6±0.2 L/h/kg), CLd/F (1.4±0.5 L/h/kg), Vc/F (1.4±0.9 L/kg), and Vp/F (4.8±2.4 L/kg). (R)-albuterol administration was associated with an increase in the dogs heart rates. A tolerance effect related to the cumulative dose was observed and modeled.
Conclusions. The presented PK-PD model appears to differentiate gut from lung absorption when (R)-albuterol is given by 15-minute nebulization to dogs. These results agree with the accepted hypothesis that most of the systemic exposure of (R)-albuterol after nebulized administration is due to gut absorption.
Similar content being viewed by others
REFERENCES
R. C. Ahrens and G. D. Smith. Albuterol: An adrenergic agent for use in the treatment of asthma. Pharmacology, pharmacokinetics and clinical use. Pharmacotherapy 4:105–120 (1984).
D. W. Boulton and J. P. Fawcett. Enantioselective disposition of salbutamol in man following oral and intravenous administration. Br. J. Clin. Pharmacol. 41:35–40 (1996).
D. W. Boulton and J. P. Fawcett. Pharmacokinetics and pharmacodynamics of single oral doses of albuterol and its enantiomers in humans. Clin. Pharmacol. Ther. 62:138–144 (1997).
E. A. Eaton, U. K. Walle, H. M. Wilson, G. Aberg, and T. Walle. Stereoselective sulphate conjugation of salbutamol by human lung and bronchial epithelial cells. Br. J. Clin. Pharmacol. 41:201–206 (1996).
I. W. Wainer. Three-dimensional view of pharmacology. Am. J. Hosp. Pharm. 49 (Suppl. 1):S4–8 (1992).
A. C. Penna and K. P. Dawson. Nebulized salbutamol (albuterol): Systemic absorption could be important in achieving bronchodilatation. J. Asthma 30:105–107 (1993).
K. M. Fried, P. Koch, and I. W. Wainer. Determination of the enantiomers of albuterol in human and canine plasma by enantioselective high-performance liquid chromatography on a teicoplanin-based chiral stationary phase. Chirality 10:484–491 (1998).
M. Gibaldi and D. Perrier. Pharmacokinetics, 2nd ed. Marcel Dekker, New York, 1982.
B. Meibohm and H. Derendorf. Basic concepts of pharmacokinetic/pharmacodynamic (PK/PD) modelling. Int. J. Clin. Pharmacol. Ther. 10:401–413 (1997).
D. Z. D'Argenio and A. Schumitzky. ADAPT-II Users Manual. Biomedical Simulations Resource, University of Southern California, Los Angeles, 1997.
D. Collins and A. Forrest. IT2S user's guide. State University of New York at Buffalo, Buffalo, 1995.
A. Forrest, C. H. Ballow, D. E. Nix, M. C. Birmingham, and J. J. Schentag. Development of a population pharmacokinetic model and optimal sampling strategies for intravenous ciprofloxacin. Antimicrob. Agents Chemother. 37:1065–1072 (1993).
J. L. Steimer, A. Mallet, J. L. Golmar, and J. F. Boivieux. Alternative approaches to estimation of population pharmacokinetic parameters: Comparison with the nonlinear mixed-effect model. Drug Metab. Rev. 15:265–292 (1984).
G. M. Shenfield, M. E. Evans, S. R. Walker, and J. W. Paterson. The fate of nebulized salbutamol (albuterol) administered by intermittent positive pressure respiration to asthmatic patients. Am. Rev. Respir. Dis. 108:501–505 (1973).
G. M. Shenfield, M. E. Evans, and J. W. Paterson. The effect of different nebulizers with and without intermittent positive pressure breathing on the absorption and metabolism of salbutamol. Br. J. Pharmacol. 1:295–300 (1974).
C. Janson. Plasma levels and effects of salbutamol after inhaled or i.v. administration in stable asthma. Eur. Respir. J. 4:544–550 (1991).
H. T. Nilsson, B. G. Simonsson, and B. Ström. The fate of 3H-terbutaline sulphate administered to man as an aerosol. Eur. J. Clin. Pharmacol. 10:1–7 (1976).
D. S. Davies. The fate of inhaled terbutaline. Eur. J. Resp. Dis. 65(Suppl 134):141–147 (1984).
M. G. M. Derks, B. T. J. van den Berg, J. S. van der Zee, M. C. P. Braat, and C. J. van Boxtel. Biphasic effect-time courses in man after formoterol inhalation: Eosinopenic and hypokaliemic effects and inhibition of allergic skin reactions. J. Pharmacol. Exp. Ther. 283:824–832 (1997).
K. Gumbhir-Shah, D. J. Kellerman, S. DeGraw, P. Koch, and W. J. Jusko. Pharmacokinetics and pharmacodynamics of cumulative single doses of inhaled salbutamol enantiomers in asthmatic subjects. Pulm. Pharmacol. Ther. 12:353–362 (1999).
S. P. Newman, D. Pavia, F. Moren, N. F. Sheahan, and S. W. Clarke. Deposition of pressurized aerosols in the human respiratory tract. Thorax 36:52–55 (1981).
R. Melchor, M. F. Biddiscombe, V. H. F. Mak, M. D. Short, and S. G. Spiro. Lung deposition patterns of directly labelled salbutamol in normal subjects and in patients with reversible airflow obstruction. Thorax 48:506–511 (1993).
S. R. Walker, M. E. Evans, A. J. Richards, and J. W. Paterson. The clinical pharmacology of oral and inhaled salbutamol. Clin. Pharmacol. Ther. 13:861–867 (1972).
S. Perreault, L. Dumont, V. Villiere, H. Ong, A. Adam, and P. Du Souich. Hepatic and extrahepatic metabolism of salbutamol in anesthetized rabbits. Drug Metab. Dispo. 21:485–491 (1993).
G. M. Pacifici, B. Giulianetti, M. C. Quilici, R. Spisni, M. Nervi, L. Giuliani, and R. Gomeni. (-)-Salbutamol sulphation in the human liver and duodenal mucosa: interindividual variability. Xenobiotica 27:279–286 (1997).
L. E. Martin, J. C. Hobson, J. A. Page, and C. Harrison. Metabolic studies of salbutamol-3H: A new bronchodilator, in rat, rabbit, dog and man. Eur. J. Pharmacol. 14:183–199 (1971).
D. J. Morgan. Clinical pharmacokinetics of β-Agonists. Clin. Pharmacokinet. 18:270–294 (1990).
G. R. Pesola and T. Walle. Enantiomeric interaction in the sulfate conjugation of the β2-agonist drug albuterol by the human liver. Res. Commun. Chem. Pathol. Pharmacol. 75:125–128 (1992).
B. J. Lipworth, R. A. Clark, D. P. Dhillon, and D. G. McDevitt. Subsensitivity of beta-adrenoceptor responses in asthmatic patients taking regular low dose inhaled salbutamol. Eur. J. Clin. Pharmacol. 38:203–205 (1990).
D. G. White, T. P. Rolph, and A. J. Wagstaff. The effects of salbutamolon blood pressure and heart rate in large white and pietrain-cross breeds of pig. J. Vet. Pharmacol. Ther. 12:179–188 (1989).
B. J. Lipworth, A. D. Struthers, and D. G. McDevitt. Tachyphylaxis to systemic but not airway responses during prolonged therapy with high dose inhaled salbutamol in asthmatics. Am. Rev. Resp. Dis. 140:586–592 (1989).
D. W. Cockcroft, B. E. Davis, V. A. Swystun, and D. D. Marciniuk. Tolerance to the bronchoprotective effect of beta2-agonists: Comparison of the enantiomers of salbutamol with racemic salbutamol and placebo. J. Allergy Clin. Immunol. 103: 1049–1053 (1999).
J. G. Maconochie, N. A. Minton, J. E. Chilton, and O. N. Keene. Does tachyphylaxis occur to the non-pulmonary effects of salmeterol? Br. J. Clin. Pharmacol. 37:199–204 (1994).
J. W. Jenne, G. Valcarenghi, W. S. Druz, P. W. Starkey, C. Yu, and T. K. Shaughnessy. Comparison of tremor responses to orally administered albuterol and terbutaline. Am. Rev. Respir. Dis. 134:708–713 (1986).
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Auclair, B., Wainer, I.W., Fried, K. et al. A Population Analysis of Nebulized (R)-albuterol in Dogs Using a Novel Mixed Gut-Lung Absorption PK-PD Model. Pharm Res 17, 1228–1235 (2000). https://doi.org/10.1023/A:1026466730347
Issue Date:
DOI: https://doi.org/10.1023/A:1026466730347