Abstract
Objective Acute normovolaemic haemodilution with subsequent autologous blood transfusion after surgery is widely used to reduce homologous blood requirements during cardiac surgery. The hypothesis tested was whether a low intraoperative haematocrit (Hct) resulting from haemodilution decreases gastric mucosal pH (pHi).
Design Prospective clinical investigation.
Setting University Hospital of Vienna, Austria.
Patients 16 consecutive patients scheduled for elective cardiac surgery.
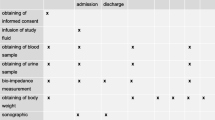
Interventions The patients were randomly assigned to one of two groups: In 10 patients (group 1), 500 ml of blood was withdrawn and stored after anaesthesia induction. An equal amount of 6 % hydroxyethyl starch was simultaneously infused. After discontinuation of cardiopulmonary bypass (CPB), the autologous blood unit was transfused. Six patients (group 2), who were not subjected to haemodilution and autologous blood transfusion served as controls. In all patients, a gastric tonometry probe was inserted.
Measurements and results Measurements of pHi and Hct were performed before and after acute normovolaemic haemodilution, during pulsatile hypothermic (30–32 °C) CPB, after rewarming, and 30 min after autologous blood transfusion in group 1, and at corresponding time intervals in group 2. Repeated measures analysis of variance and the Mann-Whitney U test were used for statistical analysis. Data are presented as means ± standard error of the mean. Haemodilution in group 1 caused a significant and persistent decrease in Hct (after haemodilution in group 1 34 ± 1 vs 40 ± 1 % in group 2). In both groups, pHi decreased during rewarming and after termination of CPB. However, in group 1, pHi was better preserved than in group 2 (rewarming: 7.44 ± 0.02 vs 7.34 ± 0.04; after CPB: 7.38 ± 0.03 vs 7.28 ± 0.02; p < 0.05).
Conclusions Acute normovolaemic haemodilution does not aggravate gastric mucosal acidosis during cardiac surgery.
Similar content being viewed by others
References
Petry AF, Jost J, Sievers H (1994) Reduction of homologous blood requirements by blood-pooling at the onset of cardiopulmonary bypass. J Thorac Cardiovasc Surg 107:1210–1214
Khan RM, Siddiqui AM, Natrajan KM (1993) Blood conservation and autotransfusion in cardiac surgery. J Card Surg 8: 25–31
Scott WJ, Rode R, Castlemain B, Kessler R, Follis F, Pett SB, Wernly JA (1992) Efficacy, complications, and cost of a comprehensive blood conservation program of cardiac operations. J Thorac Cardiovasc Surg 103: 1001–1006
Cole DJ, Drummond JC, Patel PM, Marcantonio S (1994) Effects of viscosity and oxygen content on cerebral blood flow in ischemic and normal rat brain. J Neurol Sei 124:15–20
Scott WJ, Rode R, Castlemain B, Kessler R, Follis F, Pett SB, Wernly JA (1995) The effect of cardiopulmonary bypass on intestinal and pulmonary endothelial permeability. Chest 108: 718–724
Ohri SK, Becket J, Brannan J, Keogh BE, Taylor KM (1994) Effects of cardiopulmonary bypass on gut blood flow, oxygen utilization, and intramucosal pH. Ann Thorac Surg 57:1193–1199
Tao W, Zwischenberger JB, Nguyen TT, Vertrees RA, McDaniel LB, Nutt LK, Herndon DN, Kramer GC (1995) Gut mucosal ischemia during normothermic cardiopulmonary bypass results from blood flow redistribution and increased oxygen demand. J Thorac Cardiovasc Surg 110: 819–828
Tao W, Zwischenberger JB, Nguyen TT, Vertrees RA, Nutt LK, McDaniel LB, Kramer GC (1994) Hypertonic saline/dextran for cardiopulmonary bypass reduced gut tissue water but does not improve mucosal perfusion. J Surg Res 57: 718–725
Larson MV, Ahlquist DA, Karstrom L, Sarr MG (1994) Intraluminal measurement of enteric mucosal perfusion: relationship to superior mesenteric artery flow during basal and postprandial states in the dog. Surgery 115:118–126
Tokyay R, Zeigler ST, Traber DL, Stothert JC Jr, Loick HM, Heggers JP, Herndon DN (1993) Postburn gastrointestinal vasoconstriction increases bacterial and endotoxin translocation. J Appl Physiol 74:1521–1527
Fiddian-Green RG, Baker S (1987) Predictive value of the stomach wall pH for complications after cardiac operations: comparison with other monitoring. Crit Care Med 15:153–156
Mythen MG, Webb AR (1994) Intraoperative gut mucosal hypoperfusion is associated with increased post-operative complications and cost. Intensive Care Med 20: 99–104
Doglio GR, Pusajo JF, Egurrola MA, Bonfigli GC, Parra C, Vetere L, Hernandez MS, Fernandez S, Palizas F, Gutierrez G (1991) Gastric mucosal pH as a prognostic index of mortality in critically ill patients. Crit Care Med 19:1037–1040
Buckberg GD, Beyersdorf F, Allen BS, Robertson JM (1995) Integrated myocardial management: background and initial application. J Card Surg 10: 68–89
Gys T, Hubens A, Neels H, Lauwers LF, Peeters R (1988) Prognostic value of gastric intramural pH in surgical intensive care patients. Crit Care Med 16: 1222–1224
Chang MC, Cheatham ML, Nelson LD, Rutherford EJ, Morris JA Jr (1994) Gastric tonometry supplements information provided by systemic indicators of oxygen transport. J Trauma 37: 488–994
Roumen RM, Vreudge JP, Goris RJ (1994) Gastric tonometry in multiple trauma patients. J Trauma 36: 313–316
Ohri SK, Bowles CT, Siddiqui A, Khaghani A, Keogh BE, Wright G, Yacoub MH, Taylor KM (1994) The effect of cardiopulmonary bypass on gastric and colomic mucosal perfusion: a tonometric assessment. Perfusion 9:101–108
Landow L, Phillips DA, Heard SO, Prevost D, Vandersalm TJ, Fink MP (1991) Gastric tonometry and venous oximetry in cardiac surgery patients. Crit Care Med 19:1226–1233
Desai VS, Weil MH, Tang W, Yang G, Bisera J (1993) Gastric intramural pC02 during peritonitis and shock. Chest 104:1254–1258
Desai VS, Weil MH, Tang W, Yang G, Bisera J (1996) Gastric tonometry: precision and reliability are improved by a phosphate buffered solution. Crit Care Med 1996; 24: 512–516
Knichwitz G, Mertes N, Kuhmann M (1995) Improved pC02 measurement in six standard blood gas analysers using a phosphate-buffered solution for gastric tonometry. Anaesthesia 50: 532–534
Heard SO, Helsmoortel CM, Kent JC, Shahnarian A, Fink MP (1991) Gastric tonometry in healthy volunteers: Effect of ranitidine on calculated intramural pH. Crit Care Med 19: 271–274
Boyd O, Mackay CJ, Lamb G, Bland JM, Ground RM, Bennett ED (1993) Comparison of clinical information gained from routine blood-gas analysis and from gastric tonometry for intramural pH. Lancet 341:142–146
Gardeback M, Settergren G, Ohquist G, Tiren C (1995) Effect of dopexamine on calculated low gastric intramucosal pH following valve replacement. Acta Anaesthesiol Scand 39: 599–604
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was performed at the Department of Anaesthesiology and General Intensive Care, University of Vienna, Austria. The study was financed with the department’s own financial resources. The study was presented in part at the 26th Educational & Scientific Symposium of the Society of Critical Care Medicine, 6–10 February 1997, San Diego, California, USA
Rights and permissions
About this article
Cite this article
Bacher, A., Mayer, N., Rajek, A.M. et al. Acute normovolaemic haemodilution does not aggravate gastric mucosal acidosis during cardiac surgery. Intensive Care Med 24, 313–321 (1998). https://doi.org/10.1007/s001340050573
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s001340050573