Summary
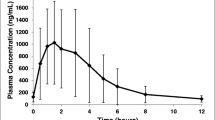
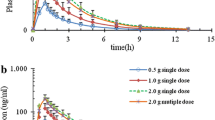
The steady state pharmacokinetics of trimethoprim was determined after 300 mg orally once daily to 6 healty volunteers for 9 days. The microbiological assay of plasma level was unreliable at trimethoprim concentrations >4 µg/ml, so results from an HPLC-assay are given. Steady state was present after 3 days. The plasma concentration peaked 1 to 4 h (mean 2.0 h) after the dose at a mean of 6.0 µg/ml (range 3.1–9.5 µg/ml); the minimum value was 1.5 µg/ml (range 0.6–2.9 µg/ml). The mean AUCss was 77 µg/ml · h and the mean plasma clearancess was 67 and 74 ml/min on Days 8 and 9. Renal clearance was about 60% of the plasma clearance. The average plasma half life was 10.6 h (range 8.7–15.3 h). Thus, there was considerable interindividual variation in all pharmacokinetic parameters. 72 h after the last dose trimethoprim was detectable in plasma in only 1 of the 6 subjects. The minimum urinary concentration of trimethoprim during treatment was always well above (range 22 to 220 µg/ml) the MIC values for most urinary tract pathogens. Therefore, a daily dose of 300 mg trimethoprim results in a therapeutic concentration in urine at steady state that lasts throughout the dosing interval and in most subjects probably lasts also for a further 24 h. Trimethoprim administration raised mean serum creatinine from 67 to 97 µmol/l, probably due to competitive inhibition of the tubular secretion of creatinine.
Similar content being viewed by others
References
Ahlmén J, Frisén J, Ekbladh G (1982) Experience of three-day trimethoprim therapy for dysuria-frequency in primary health care. Scand J Infect Dis 14: 213–216
Andrews DA, Chuter PJ, Dawson MJ, Eden BW, Moore RMA, Freestone DS, Morris CA (1981) Trimethoprim and co-trimoxazole in the treatment of acute urinary tract infections: patient compliance and efficacy. J R Coll Gen Pract 31: 274–280
Brogden RN, Carmine AA, Heel RC, Speight TM, Avery GS (1982) Trimethoprim: A review of its antibacterial activity, pharmacokinetics and therapeutic use in urinary tract infections. Drugs 23: 405–430
Brumfitt W, Hamilton-Miller IMT, Ludlam H, Damjanovic V, Gargan R (1982) Comparative trial of trimethoprim and cotrimoxazole in recurrent urinary infections. Infection 10 [5]: 280–284
Cartwright KA, Stanbrige TN, Cooper I (1982) Comparison of once daily trimethoprim and standard co-trimoxazole in urinary infections. A clinical trial in general practice. Clin Trials 226: 152–156
Craig WA, Kunin CM (1973) Trimethoprim-sulfametoxazole: pharmacodynamic effects of urinary pH and impaired renal function. Ann Int Med 78: 491–497
Editorial (1980) Trimethoprim. Lancet 1: 519–520
Gomeini C, Gomeini R (1978) IGPHARM Interactive graphic package for pharmacokinetic analysis. Computer Biomed Research 14: 345–361
Iravani A, Richard GA, Baer H (1982) Trimethoprim once daily vs. nitrofurantoin in treatment of acute urinary tract infections in young women, with special reference to periurethral, vaginal, and fecal flora. Rev Infect Dis 4: 378–387
Kainer G, Rosenberg AR (1981) Effect of co-trimoxazole on the glomerular filtration rate of healthy adults. Chemother 27: 229–232
Kasanen A, Anttila M, Elfving R, Kahela P, Saarimaa H, Sundquist H, Tikkanen R, Toivanen P (1978) Trimethoprim. Pharmacology, antimicrobial activity and clinical use in urinary tract infections. Ann Clin Res 10 [Suppl 22]: 7–13
Kremers P, Duvivier J, Heusghem C (1974) Pharmacokinetic studies of co-trimoxazole in man after single and repeated doses. J Clin Pharmacol 14: 112–118
Lee J, Hollyer R, Rodelas R, Preuss HG (1981) The influence of trimethoprim, sulfametoxazole and creatinine on renal organic anion and cation transport in rat kidney tissue. Toxicol Appl Pharmacol 58: 184–193
Light RB, Ronald AR, Harding GKM, Dikkema J, Thompson L, Buckwold FJ (1981) Trimethoprim alone in the treatment and prophylaxis of urinary tract infection. Arch Int Med 141: 1807–1810
Patel RB, Welling PG (1980) Clinical pharmacokinetics of cotrimoxazole (trimethoprim-sulphametoxazole). Clin Pharmacolkinet 5: 405–423
Schwartz DE, Ziegler WH (1969) Assay and pharmacokinetics of trimethoprim in man. Postgrad Med J [Suppl] 45: 32–37
Sharpstone P (1969) The renal handling of trimethoprim and sulphamethoxazole in man. Postgrad Med J [Suppl] 45: 38–42
Vree TB, Hekster YA, Baars AM, Damsma JE, van der Kleijn E (1978) Determination of trimethoprim and sulfamethoxazole (cotrimoxazole) in body fluids of man by means of high-performance liquid chromatography. J Chromatogr 146: 103–112
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Odlind, B., Hartvig, P., Fjellström, K.E. et al. Steady state pharmacokinetics of trimethoprim 300 mg once daily in healthy volunteers assessed by two independent methods. Eur J Clin Pharmacol 26, 393–397 (1984). https://doi.org/10.1007/BF00548773
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF00548773