Abstract
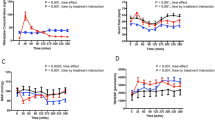
To elucidate the effect of Nicorandil on myocardial energy metabolism and myocardial sympathetic activity, we administered Nicorandil orally to eight patients with angina pectoris prior to exercise testing. Arterial and coronary sinus levels of lactate, ammonia, hypoxanthine (HX), adrenaline and noradrenaline were measured during exercise in order to determine the irrespective myocardial extraction ratios (MER). Compared to placebo, Nicorandil increased the time to development of significant ST depression (322 vs 390 s) while decreasing the maximum amplitude of ST depression (0.244 vs 0.216 mV). Heart rate, systolic blood pressure, and the rate pressure product during exercise were not significantly affected. The MER of lactate, measured during exercise, was significantly higher after Nicorandil than placebo (13.6 vs 27.9). Similarly, the MERs of ammonia and HX were significantly higher after Nicorandil (-46.0 vs 7.4% and −47.0 vs 9.9% respectively). Nicorandil, had no apparent effect on myocardial sympathetic activity as the MERs of adrenaline and noradrenaline were essentially unaffected. We conclude that Nicorandil decreased myocardial ischaemia and suppressed myocardial accelerated purine metabolism (a marker of cellular energy metabolism) during exercise in patients with angina pectoris. This effect appears not to be related to myocardial sympathetic activity.
Similar content being viewed by others
References
Preuss KC, Gross GJ, Brooks HL, Warltier DC (1985) Hemodynamic actions of nicorandil, a new antianginal agent, in the conscious dog. J Cardiovasc Pharmacol 7:709–714
Gross G, Pieper G, Farber NE, Warltier D, Hardman H (1989) Effects of nicorandil on coronary circulation and myocardial ischemia. Am J Cardiol 63:11J-17J
Gross GJ, Auchampach JA, Maruyama M, Warltier D, Pieper GM (1992) Cardioprotective effects of nicorandil. J Cardiovasc Pharmacol 20[Suppl 3]:S22-S28
Norman B, Sollevi A, Kaijser L, Jansson E (1987) ATP breakdown products in human skeletal muscle during prolonged exercise to exhaustion. Clin Physiol 7:503–509
Ketai LH, Simon RH, Kreit JW, Grum CM (1987) Plasma hypoxanthine and exercise Am Rev Respir Dis 136:98–101
Lowenstein JM, Tornheim K (1971) Ammonia production in muscle: the purine nucleotide cycle. Science 171:387–400
Mineo I, Kono N, Hara N, Shimizu T, Yamada Y, Kawachi M, Kiyokawa H, Wang YL, Tarui S (1987) Myogenic hyperuricemia: a common pathophysiologic feature of glycogenesis type III, V, and VII. N Engl J Med 317:75–80
Serruys PW, Suryapranata H, Piscione F, Harmsen E, Brand M, Feyter P, Hugenholtz PG, Jong JW (1989) Myocardial release of hypoxanthine and lactate during percutaneous transluminal coronary angioplasty. Am J Cardiol 63:45E-51E
He MX, Gorman MW, Roming GD, Sparks HV Jr (1992) Adenosine formation and myocardial energy status during graded hypoxia. J Moll Cell Cardiol 24:79–89
Smolenski RT, Suitters A, Yacoub M (1992) Adenine nucleotide catabolism and adenosine formation in isolated human cardiomyocytes. J Moll Cell Cardiol 24:91–96
Fox IH, Palella TD, Kelley WN (1987) Hyperuricemia: a marker for cell energy crisis. N Engl J Med 317:111–112
Ogino K, Kitamura H, Osaki S, Hisatome I, Miyakoda H, Matsumoto T, Noguchi N, Kinugawa T, Kotake H, Mashiba H (1993) Clinical significance of ammonia response during exercise in patients with congestive heart failure. Different implication from lactate response. J Am Coll Cardiol 21(Suppl):480A
Kosaka H, Hisatome I, Ogino K, Tanaka Y, Osaki S, Kitamura H, Omodani H, Matsumoto T, Miyakoda H, Kotake H, Mashiba H, Inoue A (1993) Excess purine degradation in muscle with chronic haemodialysis patients. Nephron 64:481–482
Ogino K, Kinugawa T, Noguchi N, Kitamura H, Matsumoto T, Miyakoda H Kotake H, Mashiba H. (1992) Suppression of sympathetic nervous system activity by Nicorandil during exercise. (1992) Gen Pharmacol 23:325–329
Andersson B, Blomström-Lundqvist C, Hedner T, Waagstein F (1991) Exercised hemodynamics and myocadial metabolism during long-term beta-blockade in severe heart failure. J Am Coll Cardiol 18:1059–1066
Borg GA (1982) Psychophysical bases of perceived exertion. Med Sci Sports Exercise 14:377–381
Kobayashi K, Hakuta T (1987) Effects of Nicorandil on coronary hemodynamics in ischemic heart disease: comparison with nitroglycerin, nifedipine, and propranolol. J Cardiovasc Pharmacol 10:S109-S115
Taira N (1989) Nicorandil as a hybrid between nitrates and potassium channel activators. Am J Cardiol 63:18J-24J
Weiss RG, Bottomley PA, Hardy CJ, Gerstenblith G (1990) Regional myocardial metabolism of high-energy phosphates during isometric exercise in patients with coronary artery disease. N Engl J Med 323:1593–1600
Lamping A, Christensen CW, Pelc LR, Warltier DC, Gross GJ (1984) Effects of nicorandil and nifedipine on protection of ischemic myocardium. J Cardiovasc Pharmacol 6:536–542
Pieper GM, Gross GJ (1987) Salutary action of Nicorandil, a new antianginal drug, on myocardial metabolism during ischemia and on postischemic function in a canine preparation of brief, repetitive coronary artery occlusions: comparison with isosorbide dinitrate. Circulation 76:916–28
Darby TD, Sprouse JH, Walton RP (1958) Evaluation of sympathetic reflex effects on the inotropic action of nitroglycerine, quinidine, papaverine, aminophylline, and isoproterenol. J Pharmacol Exp Ther 122:386–395
Nakaya H, Schwaltz A, Millard RW (1983) Reflex chronotropic and inotropic of calcium channel-blocking agents in conscious dogs. Circ Res 52:302–311
Thomas JA, Marks BH (1978) Plasma norepinephrine in congestive heart failure. Am J Cardiol. 41:233–243
Cohn JN, Levine TB, Olivari MT, Garberg V, Tura D, Francis GS, Simon AB, Rector T (1984) Plasma norepinephrine as a guide to prognosis in patients with chronic congestive heart failure. N Engl J Med 311:819–823
Swedberg K, Viquerat C, Rouleau JL, Roizen M, Atherton B, Parmely WW, Chatterjee K (1984) Comparison of myocardial catecholamine balance in chronic congestive heart failure and in angina pectoris without heart failure. Am J Cardiol 54:783–786
Kinoshita M, Nishikawa S, Sawamura M, Yamaguchi S, Mitsunami K, Itoh M, Motomura M, Bito K, Mashiro I, Kawakita S (1986) Comparative efficacy of high-dose versus low-dose Nicorandil therapy for chronic stable angina pectoris. Am J Cardiol 58:733–738
Watts JA, Norris TA, London RE, Steenbergen C, Murphy E (1990) Effects of diltiazem on lactate, ATP, and cytosolic free calcium levels in ischemic hearts. J Cardiovasc Pharmacol 15:44–49
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Ogino, K., Osaki, S., Noguchi, N. et al. Nicorandil suppressed myocardial purine metabolism during exercise in patients with angina pectoris. Eur J Clin Pharmacol 48, 189–194 (1995). https://doi.org/10.1007/BF00198297
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF00198297