Abstract
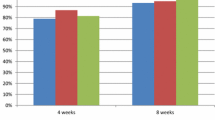
To assess the comparative efficacy of omeprazole 20 mg, a proton pump inhibitor, versus ranitidine 150 mg twice a day, an H2-receptor antagonist, in healing duodenal ulcers we performed a randomized, double-blind, multicenter trial in 309 patients with endoscopically diagnosed ulcers. Patients were treated for up to four weeks and were seen at week 2 and at week 4, if unhealed at week 2, for determination of ulcer status by endoscopy, review of daily self-assessment symptom diaries, and clinical laboratory including fasting serum gastrin. Gastrin levels were repeated two weeks after cessation of study medication. Evaluation of baseline demographic and laboratory parameters demonstrated no significant differences between the two groups at entry. At week 2, 42% of the omeprazole and 34% of the ranitidine-treated patients were healed (P=NS). At week 4, there was a 19% advantage in ulcer healing for the omeprazole-treated patients in comparison to those treated with ranitidine (82% vs 63%, respectively,P<0.05). Healing of ulcers ≥1.0 cm occurred in 83% of those treated with omeprazole versus 37% treated with ranitidine (P<0.01). There were no significant differences in rate of pain relief or incidence of clinical laboratory abnormalities. Mean fasting serum gastrin value during treatment increased over the baseline in both groups, (P<0.05). The percent change was significantly greater with omeprazole but few patients had elevations above the upper limit of normal for the assay. Both drugs were well tolerated. Omeprazole 20 mg demonstrated superiority in healing duodenal ulcers at four weeks in comparison to ranitidine 150 mg twice daily and was more effective in healing ulcers >-1.0 cm.
Similar content being viewed by others
References
Howden CW, Jones DB, Burget DW, Hunt RH: Comparison of the effects of gastric antisecretory agents in healthy volunteers and patients with duodenal ulcer. Gut 27(9):1058–1061, 1986
Jones DB, Howden CW, Burget DW, Kerr GD, Hunt RH: Acid suppression in duodenal ulcer: a meta-analysis to define optimal dosing with antisecretory drugs. Gut 28(9):1120–1127, 1987
Burget DW, Chiverton SG, Hunt RH: Is there an optimal degree of acid suppression for healing in duodenal ulcer? A model of the relationship between ulcer healing and acid suppression. Gastroenterology 99(2):345–351, 1990
Clissold SP, Campoli-Richards DM: Omeprazole: A preliminary review of its pharmacodynamic and pharmacokinetic propeties, and therapeutic potential in peptic ulcer disease and Zollinger-Ellison syndrome. Drugs 32(1):15–47, 1986
Sachs G: Pump blockers and ulcer disease. N Engl J Med 310(12):785–786, 1984
Berglindh T, Sachs G: Emerging strategies in ulcer therapy: Pumps and receptors. Scand J Gastroenterol (Suppl) 108:7–14, 1985
Naesdal J, Bodemar G, Walan A: Effect of omeprazole, a substituted benzimidazole, on 24-h intragastric acidity in patients with peptic ulcer disease. Scand J Gastroenterol 19(7):916–922, 1984
Thompson JN, Barr JA, Collier N, et al: Basal, sham feed and pentagastrin stimulated gastric acid, pepsin, and electrolytes after omeprazole 20 mg and 40 mg daily. Gut 26(10):1018–1024, 1985
Gustavsson S, Adami HO, Loof L, etal: Rapid healing of duodenal ulcers with omeprazole: Double-blind dosecomparative trial. Lancet 2(8324):124–125, 1983
Lauritsen K, Rune SJ, Bytzer P, et al: Effect of omeprazole and cimetidine on duodenal ulcer. A double-blind comparative trial. N Engl J Med 312(15):958–961, 1985
McArthur KE, Jensen RT, Gardner JD: Treatment of acid-peptic diseases by inhibition of gastric H+K+ ATPase. Annu Rev Med 37:97–105, 1986
Crobach LFSJ, Jansen JBMJ, Lamers CBHW: Effect of intermittent weekend therapy with omeprazole on basal and postprandial serum gastrin concentrations in patients with duodenal ulcer. Clin Pharmacol Ther 43(6):643–647, 1988
Solvell L: Safety aspects of omeprazole. Scand J Gastroenterol 21(Suppl 118):129–135, 1986
Betton GR, Dormer CS, Wells T, et al: Gastric ECL-cell hyperplasia and carcinoids in rodents following chronic administration of H2-antagonists SKF 93479 and oxmetidine and omeprazole. Toxicol Pathol 16(2):288–298, 1988
Helander HF: Oxyntic mucosa histology in omeprazoletreated patients suffering from duodenal ulcer of Zollinger-Ellison syndrome. Digestion 35(suppl 1):123–129, 1986
Creutzfeldt W, Lamberts R, Stockmann F, Brunner G: Quantitative studies of gastric endocrine cells in patients receiving long-term treatment with omeprazole. Scand J Gastroenterol 24(suppl 166):122–128, 1989
Solcia E, Rindi G, Havu N, Elm G: Qualititative studies of gastric endocrine cells in patients treated long-term with omeprazole. Scand J Gastroenterol 24(suppl 166):129–139, 1989
Havu N, Mattsson H, Ekman L, Carlsson E: ECL-cell carcinoids in the rat gastric mucosa following long-term administration of ranitidine. Digestion 45(4):189–195, 1990
Borch K, Renvall H, Leidberg G: Gastric endocrine cell hyperplasia and carcinoid tumors in pernicious anemia. Gastroenterology 88(3):638–648, 1985
Bardram L, Thomsen P, Stadil F: Gastric endocrine cells in omeprazole-treated and untreated patients with the Zollinger-Ellison syndrome. Digestion 35(suppl 1):116–122, 1986
McGuigan JE, Trudeau WL: Immunochemical measurement of elevated gastrin levels in the serum of patients with pancreatic tumors of the Zollinger-Ellison variety. N Engl J Med 278(24):1308–1313, 1968
Fleiss JL: The Design and Analysis of Clinical Experiments. New York, John Wiley & Sons, 1986
Wormesly KG: Assessing the safety of drugs for the long-term treatment of peptic ulcers. Gut 25(12):1416–1423, 1984
Brunner G, Creutzfeldt W, Harke U, Lamberts R: Therapy with omeprazole in patients with peptic ulcerations resistant to extended high-dose ranitidine treatment. Digestion 39(2):80–90, 1988
Ekman L, Hansson D, Havu N, Carlsson E, Lundberg C: Toxicological studies on omeprazole. Scand J Gastroenterol (Suppl) 108:53–69, 1985
Harvu N, Mattsson H, Carlsson K, Lundell L, Carlsson E, Brautigam J: Partial fundectomy results in hypergastrinemia and the development of gastric ECL cell carcinoids in the rat. Gastroenterology 96:A330, 1989
Hirschowitz BI, Griffith J, Pellegrin D, Cummings OW: Rapid regression of ECL-cell gastric carcinoids in 3 patients with pernicious anemia after elimination of hypergastrinemia by antrectomy. Gastroenterology 98:A286, 1990
Author information
Authors and Affiliations
Additional information
This work was supported by the National Institutes of Arthritis and Metabolism and Digestive Diseases grant AM34840, Veterans Administration Research Funds, and Merck, Sharp and Dohme Research Laboratories.
Rights and permissions
About this article
Cite this article
Valenzuela, J.E., Berlin, R.G., Snape, W.J. et al. U.S. experience with omeprazole in duodenal ulcer. Digest Dis Sci 36, 761–768 (1991). https://doi.org/10.1007/BF01311234
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF01311234