Summary
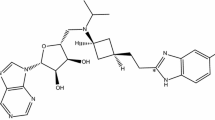
The pharmacokinetics of bendazac and its major metabolite, 5-hydroxybendazac, have been investigated in 15 patients with moderate to severe renal insufficiency and renal failure following a single oral dose of 500 mg bendazac-lysine. The pharmacokinetic parameters were compared to those obtained in 10 healthy adult volunteers.
The rate and the extent of absorption of bendazac was not modified in the patients with moderate and severe renal insufficiency, nor was there any change in plasma tmax, Cmax, apparent elimination t1/2 and AUC.
There was a significant increase in the unbound fraction of bendazac in renal failure patients undergoing haemodialysis, with a consequent increase in the apparent volume of distribution (V/F) and apparent plasma clearance (CL/F), and a decrease in plasma Cmax and AUC. Simultaneous changes of V/F and CL/F lead to an unchanged plasma t1/2 in these patients. Renal clearance (CLR) was decreased, but CL/F was not affected, since renal excretion is a minor route of elimination of bendazac.
Bendazac is mostly eliminated by metabolism to 5-hydroxybendazac, in healthy subjects >60% of a dose being excreted in urine as 5-hydroxybendazac and its glucuronide. In patients with renal insufficiency urinary excretion of 5-hydroxybendazac was decreased and the systemic availability of the metabolite (AUC), was increased about three-fold, irrespective of the degree of renal failure. Plasma 5-hydroxybendazac glucuronide accumulated according to the degree of renal insufficiency.
Overall it can be assumed that the pharmacological effect of the drug will not be enhanced in renal failure and that the dosage regimen of bendazac-lysine in such patients need not be modified.
Similar content being viewed by others
References
Barillari G (1983) Oral absorption of Bendazac-lysine salt in man after repeated administrations. Pharmacol Res Commun 15: 461–471
Berson SA, Yallow RS, Schreider SS, Pot J (1953) Tracer experiment with131I-labelled human serum albumin: Distribution and degradation studies. J Clin Invest 32: 746–768
Bonomi L, Marchini G, de Franco I, Perfetti S, de Gregorio M (1983) Bendazac lysine salt in treatment of cataract — a controlled study. Curr Ther Res Clin Esp 33: 727–732
Caramazza R, de Gregorio M, Pioggia M (1985) Valutazione clinica controllata del bendazac lisina nella cataratta senile in uno studio policentrico. Analisi dell'effetto di sei mesi di trattamento. Boll Ocul 64: 1–18
Catanese B, Barillari G, Iorio E, Silvestrini B (1982) A comparative study of the oral absorption in man of bendazac and its lysine salt. Boll Chim Farm 121: 87–90
Dettli L (1984) The kidney in pre-clinical and clinical pharmacokinetics. Jpn J Clin Pharmacol Ther 15: 241–254
Fehske KJ, Müller WE, Wollert U (1981) The location of drug binding sites in human serum albumin. Biochem Pharmacol 30: 687–692
Gambertoglio JG (1984) Effects of renal disease: Altered pharmacokinetics. In: Benet LZ, Massoud N, Gambertoglio JG (eds) Pharmacokinetic basis for drug treatment. Raven Press, New York, pp 149–171
Gomeni C, Gomeni R (1978) IGPHARM: Interactive Graphic Package for Pharmacokinetic Analysis. Comput Biomed Res 11: 345–361
Gugler R, Kurten JW, Jansen CJ, Klehr V, Hartlapp J (1979) Clofibrate disposition in renal failure and acute and chronic liver disease. Eur J Clin Pharmacol 15: 341–347
Letteri JM, Mellk H, Louis S, Kutt H, Durante P, Glazko A (1971) Diphenylhydrantoin metabolism in uremia. N Engl J Med 285: 648–652
Recupero SM, Librando A, Mannino G (1984) Valutazione clinica sull'impiego della bendalina nella terapia della cataratta. Clin Ocul Pat Oculare 5: 301–306
Reidenberg MM (1977) The biotransformation of drugs in renal failure. Am J Med 62: 482–485
Rovei V, Ego D, Catanese B (1987) Pharmacokinetic and metabolism of bendazac-lysine. Proc XXV Int Congr Ophthalm, Roma 1986. In: D'Ermo F, Ponte F, Laties AM (eds) Recent developments in the pharmacological treatment of cataract. Kugler publications. Ghedini Editore, pp 15–23
Silvestrini B, Catanese B, Barillari G, Iorio E, Valeri P (1983) Basic data supporting the use of the L-lysine salt of bendazac in cataract. Int J Tissue React 5: 217–225
Sudlow G (1978) Biochemical clinical pharmacology, vol 7. (Tillement JP ed), Pergamon Press, Paris, pp 113–123
Tozer TN (1981) Concepts basic to pharmacokinetics. Pharmacol Ther 12: 109–131
Vallner JJ (1977) Binding of drugs by albumin and plasma protein. J Pharm Sci 66: 447–465
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Rovei, V., Campistron, G., Dueymes, J.M. et al. Pharmacokinetics of bendazac-lysine and 5-hydroxybendazac in patients with renal insufficiency. Eur J Clin Pharmacol 33, 303–310 (1987). https://doi.org/10.1007/BF00637567
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF00637567