Abstract
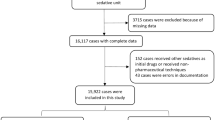
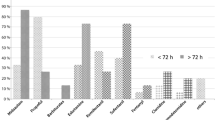
Orally administered chloral hydrate is the most widely used sedative in children undergoing MRI. We compared intermediate-and high-dose oral chloral hydrate in 97 consecutive children undergoing MRI in a prospective, controlled, double-blind, randomised clinical trial. There were 50 girls and 47 boys, mean weight (±SD) 14.7±6.4 kg, and mean age 38±31. The children were randomly allocated to receive chloral hydrate syrup either 70 mg/kg (group A,n=50) or 100 mg/kg (group B,n=47). These two groups were not significantly different in sex, weight, age, diagnosis or ambulatory medication. The mean initial dose (±SEM) was 64±2 mg/kg for group A and 93±2 mg/kg for group B. Because adequate sedation was not achieved, 14 patients in group A and 6 in group B required a second dose, giving a mean total dose of 70±2 mg/kg for group A and 96±2 mg/kg for group B. The percentage of successful examinations after the initial dose (A: 64%, B: 87%;p<0.05) and the total dose (A: 92%, B: 100%;p=0.14) was higher in group B. Significant differences were found for the time of onset of sedation (A: 28±2 min, B: 21±1 min;p<0.05), but not for the time to spontaneous awakening after the completion of the examination. The rate of adverse reactions was similar (A: 20%, B: 21%;p=1.00). We conclude that high-dose oral chloral hydrate improves the management of children undergoing MRI.
Similar content being viewed by others
References
Keeter S, Benator RM, Weinberg SM, Hartenberg MA (1990) Sedation in pediatric CT: national survey of current prastice. Radiology 175: 745–752
Anonymous (1993) USP DI. Drug information for the health care professional, vol I, 13th edn. United States Pharmacopeial Convention. Rockville, Md. pp 792–794
Gómez MR; Reese DR (1976) Computed tomography of the head in infants and children. Pediatr Clin North Am 23: 473–498
McCullough DC, Kufta C, Axelbaum SP, Schellinger D (1977) Computerized axial tomography in clinical pediatries. Pediatrics 59: 173–181
Mitchell AA, Louik C, Lacouture P, Slone D, Goldman P, Shapiro S (1982) Risks to children from computer tomographic scan premedication. JAMA 247: 2385–2388
Thompson JR, Schneider S, Ashwal S, Holden BS, Hinshaw DB, Hasso AN (1982) The choice of sedation for computed tomography in children: a prospective study. Radiology 143: 475–479
Weir MR, Segapelli JH, Tremper LJ (1986) Sedation for pediatric procedure. Mil Med 151: 181–184
Martí-Bonmatí L, Ronchera CL, Talens A, Hernández T, Vilar J, Jiménez NV (1990) Hipnosis en pacientes pediátricos estudiados con resonancia magnética: evaluatión del hidrato de cloral. Radiología 32: 383–386
Greenberg SB, Faerber EN, Aspinall CL (1991) High-dose chloral hydrate sedation for children undergoing CT. J Comput Assit Tomogr 15: 467–469
Ronchera C, Martí-Bonmatí L, Poyatos C, Vilar J, Jiménez NV (1992) Administration of oral chloral hydrate to pediatric patients undergoing magnetic resonance imaging. Pharm Weekbl Sci 14: 349–352
Hubbard AM, Markowitz RI, Kimmel B, Kroger M, Bartko MB (1992) Sedation for pediatric patients undergoing CT and MRI. J Comput Assist Tomogr 16: 3–6
Greenberg SB, Faerber EN, Aspinall CL, Adams RC (1993) High-dose chloral hydrate sedation for children undergoing MR imaging: safety and efficacy in relation to age. AJR 161: 639–641
Pereira JK, Burrows PE, Richards HM, Chuang SH, Babyn PS (1993) Comparison of sedation regimens for pediatric outpatient CT. Pediatr Radiol 23: 341–344
Slovis TL, Parks C, Reneau D, Becker CJ, Hersch J, Carver DC, et al (1993) Pediatric sedation: short-term effects. Pediatr Radiol 23: 345–348
Nahata MC (1988) Sedation in pediatric patients undergoing diagnostic procedures. Drug Intell Clin Pharm 22: 711–715
American Academy of Pediatrics, Committee on Drugs (1992) Guidelines for monitoring and management of pediatric patients during and after sedation for diagnostic and therapeutic procedures. Pediatrics 89: 1110–1115
Strain JD, Harvey LA, Foley LC, Campbell JB (1986) Intravenously administered ministered pentobarbital sodium for sedation in pediatric CT. Radiology 161: 105–108
Fisher DM (1990) Sedation of pediatric patients: an anesthesiologist's perspective. Radiology 175: 613–615
Mitchell AA, Louik C, Lacouture PG, Goldman P, Shapiro S (1983) Computer tomographic premedication in children (letter). JAMA 249: 2639
Bisset GS, Ball WS (1991) Preparation, sedation, and monitoring of the pediatric patient in the magnetic resonance suite. Semin Ultrasound CT MR 12: 376–378
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Martí-Bonmatí, L., Ronchera-Oms, C.L., Casillas, C. et al. Randomised double-blind clinical trial of intermediate- versus high-dose chloral hydrate for neuroimaging of children. Neuroradiology 37, 687–691 (1995). https://doi.org/10.1007/BF00593395
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF00593395