Abstract
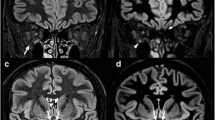
Fast spin-echo (FSE) is a new sequence with acquisition times currently down to one-sixteenth of those obtained with conventional spin-echo sequences, which allows high-resolution (512×512 matrix) images to be acquired in an acceptable time. We compared the higher resolution of FSE with the medium resolution of a short inversion-time inversion-recovery (STIR) sequence in depicting the optic nerves of healthy controls and patients with optic neuritis. Optic nerve MRI examinations were performed in 18 patients with optic neuritis and 10 normal controls. Two sequences were obtained coronally: fat-suppressed FSE (FSE TR 3250 ms/TEef 68 ms, echo-train length 16, 4 excitations, 24 cm rectangular field of view, 3 mm interleaved contiguous slices, in-plane resolution 0.5×0.5 mm) and STIR (TR 2000 ms/TE 50 ms/TI 175 ms, inplane resolution 0.8×0.8 mm, slice thickness 5 mm). FSE demonstrated much more anatomical detail than STIR, e. g. distinction of optic nerve and sheath. Lesions were seen in 20 of 21 symptomatic nerves using FSE and in 18 of 21 using STIR. Nerve swelling or partial cross-sectional lesions of the optic nerve were each seen only on FSE in 3 cases. Fatsuppressed FSE imaging of the optic nerve improves anatomical definition and increases lesion detection in optic neuritis.
Similar content being viewed by others
References
Halliday AM (1982) Evoked potentials in clinical testing. Churchill Livingstone, Edinburgh
Mathews WB (1991) McAlpine's multiple sclerosis. 2nd edn. Churchill Livingstone, Edinburgh
Francis DA, Compston DAS, Batchelor JR, McDonald WI (1987) A reassessment of the risk of multipie sclerosis developing in patents with optic neuritis after extended follow-up. J Neurol Neurosurg Psychiatry 50: 758–765
Youl BD, Turano G, Miller DH, et al (1991) The pathophysiology of optic neuritis. Brain 114:2437–2450
Johnson G, Miller DH, MacManus DG, et al (1987) STIR sequences in NMR imaging of the optic nerve. Neuroradiology 29:238–245
Miller DH, Newton MR, Poel JC van der et al (1988) Magnetic resonance imaging of the optic nerve in optic neuritis. Neurology 38:175–179
Miller DH, MacManus DG, Barlett PA, et al (1993) Detection of optic nerve lesions in optic neuritis using frequency-selective fat-saturation sequences. Neuroradiology 35:156–158
Simon J, Szumowski J, Totermann S, et al (1988) Fat suppression MRI of the orbit AJNR 9:961–968
Hennig J, Naureth A, Friedburg H (1986) RARE imaging: a fast imaging method for clinical MR. Magn Reson Med 3:823–833
Constable RT, Anderson AW, Zhong J, et al (1992) Factors influencing contrast in fast spin-ech MR imaging. Magn Reson Imaging 10:497–511
Kidd D, Thorpe JW, Kendall BE, et al (1993) Spinal cord MRI using multi-array coils and fast spin echo. 1. Findings in multiple sclerosis. Neurology 43: 2632–2637
McDonald WI, Barnes D (1989) Lessons from magnetic resonance imaging in multiple sclerosis. Trends Neurol Sci 12:376–379
McCrary JA, Demer JC, Friedman DI, Mawad MM (1987) Computed tomography and magnetic resonance imaging in the diagnosis of inflammatory disease of the optic nerve. Surv Opthalmol 31: 352–355
Rizzo JF, Lessell S (1991) Optic neuritis and ischemic optic neuropathy. Overlapping clinical profiles. Arch Ophthalmol 109:1668–1672
Samples JR, Younge BR (1981) Tobacco-alcohol amblyopia. J Clin Neuroophthalmol 1:213–216
Kermode A, Miller DH (1989) MRI of tobacco-alcohol amblyopia. J Neurol Neurosurg Psychiatry 52:1447
Gass A, Barker GJ, MacManus DG, et al (1995) High resolution magnetic resonance imaging of the anterior visual pathways in patients with optic neuropathies using fast spin echo and phased array local coils. J Neurol Neurosurg Psychiatry 58:562–569
Dousset V, Grossman R, Ramer KN, et al (1992) Experimental allergic encephalomyelitis and multiple sclerosis: lesion characterization with magnetization transfer imaging. Radiology 182: 483–491
Gass A, Barker GJ, Kidd D, et al (1994) Coprrelation of magnetisation transfer ratio with clinical disability in multiple sclerosis. Ann Neurol 36:62–67
Davie CA, Hawkins CP, Baker GJ, et al (1994) Serial proton magnetic resonance spectroscopy in acute multiple sclerosis. Brain 117:49–58
Arnold DL, Matthews PM, Francis G, Antel J (1990) Proton magnetic resonance spectroscopy of human brain in vivo in the evaluation of multiple sclerosis: assessment of the load of disease. Magn Reson Med 14:154–159
Barnes D, Munro PMG, Youl BD, et al (1991) The longstanding MS lesion. A quantitative MRI and electron microscope study. Brain 114:1271–1280
Thorpe JW, Barker GJ, Jones SJ, et al (1995) Magnetisation transfer ratios and transverse magnetisation decay curves in optic neuritis: correlation with clinical findings and electrophysiology. J Neurol Neurosurg Psychiatry 59:487–492
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Gass, A., Moseley, I.F., Barker, G.J. et al. Lesion discrimination in optic neuritis using high-resolution fat-suppressed fast spin-echo MRI. Neuroradiology 38, 317–321 (1996). https://doi.org/10.1007/BF00596577
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF00596577